What is heartworm disease?
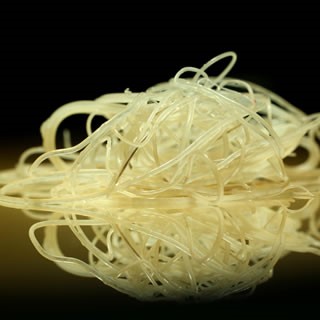
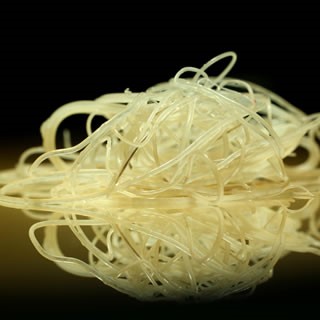
Heartworm disease is a serious and potentially fatal disease in pets in the United States and many other parts of the world. It is caused by foot-long worms (heartworms) that live in the heart, lungs and associated blood vessels of affected pets, causing severe lung disease, heart failure and damage to other organs in the body. Heartworm disease affects dogs, cats and ferrets, but heartworms also live in other mammal species, including wolves, coyotes, foxes, sea lions and—in rare instances—humans. Because wild species such as foxes and coyotes live in proximity to many urban areas, they are considered important carriers of the disease.
Dogs. The dog is a natural host for heartworms, which means that heartworms that live inside the dog mature into adults, mate and produce offspring. If untreated, their numbers can increase, and dogs have been known to harbor several hundred worms in their bodies. Heartworm disease causes lasting damage to the heart, lungs and arteries, and can affect the dog’s health and quality of life long after the parasites are gone. For this reason, prevention is by far the best option, and treatment—when needed—should be administered as early in the course of the disease as possible.
Cats. Heartworm disease in cats is very different from heartworm disease in dogs. The cat is an atypical host for heartworms, and most worms in cats do not survive to the adult stage. Cats with adult heartworms typically have just one to three worms, and many cats affected by heartworms have no adult worms. While this means heartworm disease often goes undiagnosed in cats, it’s important to understand that even immature worms cause real damage in the form of a condition known as heartworm associated respiratory disease (HARD). Moreover, the medication used to treat heartworm infections in dogs cannot be used in cats, so prevention is the only means of protecting cats from the effects of heartworm disease.
How is heartworm disease transmitted from one pet to another?
The mosquito plays an essential role in the heartworm life cycle. Adult female heartworms living in an infected dog, fox, coyote, or wolf produce microscopic baby worms called microfilaria that circulate in the bloodstream. When a mosquito bites and takes a blood meal from an infected animal, it picks up these baby worms, which develop and mature into “infective stage” larvae over a period of 10 to 14 days. Then, when the infected mosquito bites another dog, cat, or susceptible wild animal, the infective larvae are deposited onto the surface of the animal’s skin and enter the new host through the mosquito’s bite wound. Once inside a new host, it takes approximately 6 months for the larvae to mature into adult heartworms. Once mature, heartworms can live for 5 to 7 years in dogs and up to 2 or 3 years in cats. Because of the longevity of these worms, each mosquito season can lead to an increasing number of worms in an infected pet.
What are the signs of heartworm disease in dogs?
In the early stages of the disease, many dogs show few symptoms or no symptoms at all. The longer the infection persists, the more likely symptoms will develop. Active dogs, dogs heavily infected with heartworms, or those with other health problems often show pronounced clinical signs.
Signs of heartworm disease may include a mild persistent cough, reluctance to exercise, fatigue after moderate activity, decreased appetite, and weight loss. As heartworm disease progresses, pets may develop heart failure and the appearance of a swollen belly due to excess fluid in the abdomen. Dogs with large numbers of heartworms can develop a sudden blockages of blood flow within the heart leading to a life-threatening form of cardiovascular collapse. This is called caval syndrome, and is marked by a sudden onset of labored breathing, pale gums, and dark bloody or coffee-colored urine. Without prompt surgical removal of the heartworm blockage, few dogs survive.
What are the signs of heartworm disease in cats?
Signs of heartworm disease in cats can be very subtle or very dramatic. Symptoms may include coughing, asthma-like attacks, periodic vomiting, lack of appetite, or weight loss. Occasionally an affected cat may have difficulty walking, experience fainting or seizures, or suffer from fluid accumulation in the abdomen. Unfortunately, the first sign in some cases is sudden collapse of the cat, or sudden death.
How significant is my pet’s risk for heartworm infection?
Many factors must be considered, even if heartworms do not seem to be a problem in your local area. Your community may have a greater incidence of heartworm disease than you realize—or you may unknowingly travel with your pet to an area where heartworms are more common. Heartworm disease is also spreading to new regions of the country each year. Stray and neglected dogs and certain wildlife such as coyotes, wolves, and foxes can be carriers of heartworms. Mosquitoes blown great distances by the wind and the relocation of infected pets to previously uninfected areas also contribute to the spread of heartworm disease (this happened following Hurricane Katrina when 250,000 pets, many of them infected with heartworms, were “adopted” and shipped throughout the country).
The fact is that heartworm disease has been diagnosed in all 50 states, and risk factors are impossible to predict. Multiple variables, from climate variations to the presence of wildlife carriers, cause rates of infections to vary dramatically from year to year—even within communities. And because infected mosquitoes can come inside, both outdoor and indoor pets are at risk.
For that reason, the American Heartworm Society recommends that you “think 12:” (1) get your pet tested every 12 months for heartworm and (2) give your pet heartworm preventive 12 months a year.
What do I need to know about heartworm testing?
Heartworm disease is a serious, progressive disease. The earlier it is detected, the better the chances the pet will recover. There are few, if any, early signs of disease when a dog or cat is infected with heartworms, so detecting their presence with a heartworm test administered by a veterinarian is important. The test requires just a small blood sample from your pet, and it works by detecting the presence of heartworm proteins. Some veterinarians process heartworm tests right in their hospitals while others send the samples to a diagnostic laboratory. In either case, results are obtained quickly. If your pet tests positive, further tests may be ordered.
When should my pet be tested?
Testing procedures and timing differ somewhat between dogs and cats.
Dogs. All dogs should be tested annually for heartworm infection, and this can usually be done during a routine visit for preventive care. Following are guidelines on testing and timing:
· Puppies under 7 months of age can be started on heartworm prevention without a heartworm test (it takes at least 6 months for a dog to test positive after it has been infected), but should be tested 6 months after your initial visit, tested again 6 months later and yearly after that to ensure they are heartworm-free.
· Adult dogs over 7 months of age and previously not on a preventive need to be tested prior to starting heartworm prevention. They, too, need to be tested 6 months and 12 months later and annually after that.
· You need to consult your veterinarian, and immediately re-start your dog on monthly preventive—then retest your dog 6 months later. The reason for re-testing is that heartworms must be approximately 7 months old before the infection can be diagnosed.
Annual testing is necessary, even when dogs are on heartworm prevention year-round, to ensure that the prevention program is working. Heartworm medications are highly effective, but dogs can still become infected. If you miss just one dose of a monthly medication—or give it late—it can leave your dog unprotected. Even if you give the medication as recommended, your dog may spit out or vomit a heartworm pill—or rub off a topical medication. Heartworm preventives are highly effective, but not 100 percent effective. If you don’t get your dog test, you won’t know your dog needs treatment.
Cats. Heartworm infection in cats is harder to detect than in dogs, because cats are much less likely than dogs to have adult heartworms. The preferred method for screening cats includes the use of both an antigen and an antibody test (the “antibody” test detects exposure to heartworm larvae). Your veterinarian may also use x-rays or ultrasound to look for heartworm infection. Cats should be tested before being put on prevention and re-tested as the veterinarian deems appropriate to document continued exposure and risk. Because there is no approved treatment for heartworm infection in cats, prevention is critical.
What happens if my dog tests positive for heartworms?
No one wants to hear that their dog has heartworm, but the good news is that most infected dogs can be successfully treated. The goal is to first stabilize your dog if he is showing signs of disease, then kill all adult and immature worms while keeping the side effects of treatment to a minimum.
Here’s what you should expect if your dog tests positive:
· Confirm the diagnosis. Once a dog tests positive on an antigen test, the diagnosis should be confirmed with an additional—and different—test. Because the treatment regimen for heartworm is both expensive and complex, your veterinarian will want to be absolutely sure that treatment is necessary.
· Restrict exercise. This requirement might be difficult to adhere to, especially if your dog is accustomed to being active. But your dog’s normal physical activities must be restricted as soon as the diagnosis is confirmed, because physical exertion increases the rate at which the heartworms cause damage in the heart and lungs. The more severe the symptoms, the less activity your dog should have.
· Stabilize your dog’s disease. Before actual heartworm treatment can begin, your dog’s condition may need to be stabilized with appropriate therapy. In severe cases of heartworm disease, or when a dog has another serious condition, the process can take several months.
· Administer treatment. Once your veterinarian has determined your dog is stable and ready for heartworm treatment, he or she will recommend a treatment protocol involving several steps. The American Heartworm Society has guidelines for developing this plan of attack. Dogs with no signs or mild signs of heartworm disease, such as cough or exercise intolerance, have a high success rate with treatment. More severe disease can also be successfully treated, but the possibility of complications is greater. The severity of heartworm disease does not always correlate with the severity of symptoms, and dogs with many worms may have few or no symptoms early in the course of the disease.
· Test (and prevent) for success. Approximately 6 months after treatment is completed, your veterinarian will perform a heartworm test to confirm that all heartworms have been eliminated. To avoid the possibility of your dog contracting heartworm disease again, you will want to administer heartworm prevention year-round for the rest of his life.
What if my cat tests positive for heartworms?
Like dogs, cats can be infected with heartworms. There are differences, however, in the nature of the disease and how it is diagnosed and managed. Because a cat is not an ideal host for heartworms, some infections resolve on their own, although these infections can leave cats with respiratory system damage. Heartworms in the circulatory system also affect the cat’s immune system and cause symptoms such as coughing, wheezing and difficulty breathing. Heartworms in cats may even migrate to other parts of the body, such as the brain, eye and spinal cord. Severe complications such as blood clots in the lungs and lung inflammation can result when the adult worms die in the cat’s body.
Here’s what to expect if your cat tests positive for heartworm:
· Diagnosis. While infected dogs may have 30 or more worms in their heart and lungs, cats usually have 6 or fewer—and may have just one or two. But while the severity of heartworm disease in dogs is related to the number of worm, in cats, just one or two worms can make a cat very ill. Diagnosis can be complicated, requiring a physical exam, an X-ray, a complete blood count and several kinds of blood test. An ultrasound may also be performed.
· Treatment. Unfortunately, there is no approved drug therapy for heartworm infection in cats, and the drug used to treat infections in dogs is not safe for cats. Nevertheless, cats with heartworm disease can often be helped with good veterinary care. The goal is to stabilize your cat and determine a long-term management plan.
· Monitor your cat. Heartworm-positive cats may experience spontaneous clearing of heartworms, but the damage they cause may be permanent. If your cat is not showing signs of respiratory distress, but worms have been detected in the lungs, chest X-rays every 6 to 12 months may be recommended. If mild symptoms are noted, small doses of prednisolone may be administered to help reduce inflammation.
· Provide veterinary care. If the disease is severe, additional support may be necessary. Your veterinarian my recommend hospitalization in order to provide therapy, such as intravenous fluids, drugs to treat lung and heart symptoms, antibiotics, and general nursing care. In some cases, surgical removal of heartworms may be possible.
· Maintain prevention. A cat that has developed heartworm disease has demonstrated that it is susceptible to heartworm infection, and both outdoor and indoor cats are at risk. It’s important to give your cat monthly heartworm preventives, which are available in both spot-on and pill form. Preventives keep new infections from developing if an infected mosquito bites your cat again.
The age of the dog is just one factor affecting the success of heartworm treatment. When making a diagnosis and administering treatment, veterinarians consider the dog’s overall health and the severity of his symptoms, as well as the results of X-rays and laboratory test results. Older dogs with long-term heartworm infections may have damage to their lungs, hearts, livers, and kidneys that can complicate heartworm treatment. To ensure the best chance of success, it is vital to follow your veterinarian’s instructions carefully. This includes severely restricting the dog’s activity, as exercise during the treatment period is the leading cause of complications.
After treating a dog with melarsomine injections, adult worms may continue to die for more than a month following this treatment. Heartworm antigen testing is the most reliable method of confirming that all of the adult heartworms have been eliminated. Although many dogs are antigen-negative 16 weeks after treatment, it can take longer for the antigen to be completely cleared from some dogs. Additionally, even though melarsomine is highly effective, a single course of treatment may not completely clear all dogs of infection (the American Heartworm Society protocol calls for three separate injections of melarsomine. Consequently, in most cases, a dog that is still antigen positive at 4 months should be rechecked 2 to 3 months later before determining whether there are still adult heartworms remaining, and a second treatment course may be required.